What is medically assisted weight loss?
Medically assisted weight loss is a form of weight loss treatment that is given under the supervision of a medical professional. In some cases, such as here at Paragon Health Partners, this medical professional will be a board-certified obesity medicine doctor or nurse practitioner. Physicians provide weight loss treatment through nutrition and exercise education, prescription medications to help reduce hunger and cravings and promote weight loss and provide supervision throughout treatment. The type of weight loss medication and dosage is determined by your doctor after going over an extensive medical history and analysis. A medically assisted weight loss program may include or recommend a nutritionist or health coach to provide you with further in-depth coaching on how to develop healthy habits to promote weight loss. The combination of forming healthy habits through nutrition and exercise with prescribed medication from a weight loss specialized physician can be a great option for individuals struggling to lose weight on their own.
Who is eligible for medically assisted weight loss?
In simple terms, individuals with these characteristics may be eligible for weight loss:
- Individuals with a BMI of over 30
- Individuals with a BMI of over 27 with comorbidities
Individuals considered obese or individuals considered overweight who suffer from comorbidities are ideal patients for a medically assisted weight loss program. Individuals with a BMI of over 25 are considered “overweight”, and individuals with a BMI of over 30 are considered “obese”. Your BMI is a calculation based on your height and weight. A healthy BMI is considered by the CDC to be in the range of 18.5-24.9. If you are not quite obese (30 BMI and above), but you aren’t in the healthy range (18.5-24.9), with a BMI of 27 or above, you can still qualify for a medically assisted weight loss program if you suffer from comorbidities. What are comorbidities?
Comorbidities refer to the existence of more than one disease or condition, mental or physical, in the body at one time. Common diseases and conditions seen in adult Americans include diabetes, hypertension, heart disease, high cholesterol, depression, obesity, cancer, arthritis, and respiratory disease. Many of these diseases can co-occur because one may increase the likelihood of developing another. For that reason, those with an overweight BMI are eligible to participate, as their comorbidities cause a greater risk for health problems, and losing excess weight will provide many benefits in respect to health and potentially prevent additional comorbidities from developing, such as type II diabetes. It is important to treat excess weight before it leads to other conditions in the body.
With that in mind, medical weight loss is analyzed on a case-by-case basis, so it is important to schedule an initial consultation with a physician to determine whether medical weight loss is the right option for you.

How much does medical weight loss cost?
Thankfully, the answer to this question is a lot less expensive than it used to be. This is due to a recent change in legislature that has made efforts to recognize obesity as a medical condition and provide appropriate treatment to patients. This change is legislature was made in 2010, with the Affordable Care Act. The Affordable Care Act includes several provisions that aim to promote preventative care, which includes obesity screening and treatment. This means that most insurance companies are required to provide coverage for weight loss treatment options to patients with a certain BMI, or a combination of excess weight with comorbidities.
Due to this significant change in legislature, there has been a rise in options for weight loss treatment in the medical field during recent years. Now that healthcare providers can provide these services through insurance; a whole new world of weight loss options is available to patients seeking help. This is lifechanging news for those who have struggled to lose weight on their own and who seek affordable options covered by their health insurance. Weight loss treatment covered by insurance can be found in various settings with various types of healthcare providers:
- Primary care providers
- Telemedicine
- Board-certified Obesity Medicine Doctors
- Dietitians
- Nurse Practitioners
- Certified Health Coaches
- Nutritional Counselor/Therapist
Coverage varies from plan to plan and may look different depending on the state. We also provide an accessible self-pay option for patients without coverage.
What is the initial consultation like?
During the initial consultation, you will first take vitals, initial biometric measurements including body fat percentage, body measurements, and weight. You will then meet with your physician for 45-60 minutes to go over a history of present illness where you discuss your history regarding previous health conditions, weight loss attempts, and other health concerns you may have. You will then discuss your medication profile with your physician, and make sure that none of your current medications may be a factor in weight gain and if so, discuss what steps can be taken. They will also discuss medications with you to make sure none will interfere with any medications they may prescribe to you for weight loss treatment.
It is very important to go through your medical history with you in detail in order to understand you as a whole person, instead of just a number on the scale. The physician will evaluate your current habits, individual needs and personal goals you wish to achieve throughout the weight loss program. This will allow them to form a unique treatment plan for you that does not feel unattainable. They will provide you with the proper tools in order to be successful in the program. Your provider will analyze your preferences and medical history to provide a personalized meal plan that when followed properly, will promote weight loss. Your meal plan is designed to fit your needs and preferences. It is meant to be incorporated into a lifestyle that you can see yourself carrying out for the long term. It is not meant to be boring, restrictive, or difficult. This initial evaluation will give you the confidence and tools to begin your journey towards better health.
What are the steps of a medical weight loss program?
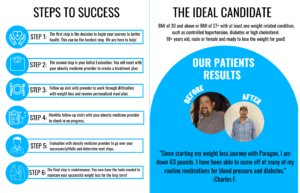
The first step is simpler than you think…
- Deciding to take the first step
This is one of the most important and in many cases, THE most important step. There are many reasons one might struggle to take this first step. In some cases, it may be the excuse of “I don’t have time.” We are constantly running from one place to another, feeling like we can’t catch up. Whether it’s work or school or kids, we always seem to find a reason to put our health at the end of our priority list. We are in a constant state of hurry and in search of anything that can make our lives feel more convenient and less stressful. Where do we normally end up cutting corners? With our own health. However, without our health, we are unable to do anything. And cutting corners for years can lead to detrimental health outcomes. Prioritizing your health is the first step. Once you make that decision, your life has the potential to change for the better. - Initial evaluation
The initial evaluation will be your initial consultation explained in detail above. This visit is the beginning of your journey to successful weight loss and improved overall health. - Follow up visits with physician
After the initial evaluation, you will have follow-up visits with your provider. These visits may be as frequent as once a week to once a month, depending on the program. In these visits, your medical provider will refill prescriptions when necessary and make sure you are satisfied with your personalized treatment plan. They want to make sure that they are provided with all the tools needed for success in the program. They will give you a personalized meal plan to fit your unique nutritional needs and preferences. They will provide guidance on how to curb cravings, portion control, meal prep, and grocery shop. They will provide education on nutrition, exercise, and healthy habit-forming skills. They will help you overcome any roadblocks or stagnancy with your weight loss. Health coaching is a crucial component to successful weight loss. It is important not only to stay on track while receiving medical weight loss treatment, but also to continue these healthy habits after you have completed the program and are no longer receiving treatment. This helps to ensure that your weight loss is a long-term outcome, and not a quick fix that lasts only a few months. It is important to establish healthy habits that you can sustain for the long term and find a lifestyle that you enjoy that promotes good health and maintenance of your weight loss. They will discuss any potential roadblocks you are experiencing and help you find a way to overcome them. A medically assisted weight loss program is meant to provide you with the helping hand and tools you need to achieve long term weight loss. - Evaluation for next steps
After 6 months of treatment, your provider will evaluate what is the best next step for you. If you have achieved successful weight loss, your provider will consider reducing or terminating your prescription if they see fit. They will also make sure you have the proper education to maintain your weight loss for the long term.In the case that you have not attained the weight loss you desired; your provider will evaluate whether you would benefit from continued medical weight loss treatment. They will analyze your pitfalls in the program and analyze reasons why you haven’t seen adequate weight loss and try to solve these issues.
In some cases, your medical provider may recommend bariatric surgery. Individuals with a BMI of over 35 or 40 with additional health conditions may be good candidates for this option. In this case, your provider would refer you to a bariatric surgeon.
- Maintenance
If your medical provider decides that you have achieved adequate weight loss and determines that you would no longer benefit from continued treatment, you have now reached the last step: maintenance. This in some cases can be the most difficult step. Throughout the program, you will be given extensive education on nutrition, exercise, and healthy habit-forming skills. These will work in conjunction with your prescribed medications to promote weight loss, as the medication will reduce hunger and cravings and allow for you to make healthier decisions. This is why it is so important to work with your provider to find a healthy lifestyle that works for you. You must find a way of eating and exercise routine that you can see yourself pursuing for the long term. The medications will not work without these elements. If you do not solidify these new habits into your life, it will be easy to go back to old habits once off the medications.Many patients benefit from support from family and friends. Long-term success can increase if other members of the household also adopt healthy changes regarding their eating and exercise habits. Medical weight loss is not a quick-fix solution. It is a tool that is used to help develop long-term habits and lifestyle changes. This is how you will see long term results and keep the weight from creeping back on. It is normal to see minimal weight gain after discontinuing the medication, but only in small amounts and only immediately after stopping the medication. Make sure that you work with your provider to find a lifestyle that works for you.
Common mistakes with medical weight loss
- Not meal planning
This is the most likely cause of unsuccessful results in the weight loss program. Nutrition is the key component in successful weight loss. If you aren’t planning your meals in advance and following your personalized calorie limit, you may not see results. Your obesity medicine provider will provide you with a meal plan customized to your needs, and your calorie limit which will lead to weight loss. Every individual requires a distinct amount of calories per day, and a specific amount to achieve a calorie deficit, which is what leads to weight loss. If you are slightly passing your daily allotted calorie amount each day, you will not see weight loss. It is important to measure the proper portion sizes in order to stay within your daily limit. A kitchen scale is the most useful tool in making sure your portion sizes follow your meal plan. Apps such as MyFitnessPal will also help you to stay on track with your meal and calorie tracking goals. - Skipping meals or undereating
If you start to skip meals, with or without the intention of losing weight, your body may go into “starvation mode.” When this happens, your metabolism slows down in order to conserve the energy that you have as a means to survive, because your body doesn’t know when it’s next meal will be. The slower your metabolism is, the less calories your body burns each day for everyday functions. This can also lead to binge eating. If you go all day without eating, and at 6pm you finally give yourself the time to eat, you might eat those 1500 calories your body needs in one session, versus spreading them out to 3, 500 calorie meals throughout the day. Since your metabolism may have slowed down due to skipping meals, eating 1500 calories will no longer be a deficit, and may even be a surplus and cause weight gain, because the body is trying to conserve any energy (food) it receives.Create a routine and eating schedule. Stay consistent with this routine. It is not necessary to skip meals or undereat in order to achieve a calorie deficit. Make sure to incorporate healthy protein, carbs, and fat throughout the day. Always go for multiple smaller meals instead of 1 huge meal. Meal prepping can really help with this, especially if you have a busy schedule. This will help prevent excuses when it comes to consistent mealtimes while also maintaining a healthy diet and not going for a quick fix like fast food.
- Ignoring stress levels
Stress is a key factor in weight gain. We tend to highly underestimate the negative effects that stress can have on our health. Stress is associated with obesity, and the neurobiology of stress overlaps significantly with that of appetite and energy regulation. Increasing levels of weight above healthy levels and the overeating of highly palatable foods results in changes of glucose metabolism, insulin sensitivity and hormones regulating appetite and energy homeostasis. “These metabolic factors not only influence neural reward regions to impact motivation, but also affect hypothalamic circuits, interacting with the overlapping stress and energy regulation circuitry.” (1) There is plenty of research that displays evidence of stress being tied to obesity. This is why it is so important to address high stress levels and find ways to reduce them. This may be through exercise, walking, sports, hobbies, meditating, journaling, you name it. Find what stress reducing activities work best for you and make sure to prioritize the time for them. - Inadequate sleep
Sleep is another highly underestimated factor in weight gain. Seven to nine hours of sleep a night is considered appropriate to support good health in adults of 18–60 years of age. Disturbed sleeping patterns lead to increased energy intake, partly from excessive snacking, mainly on foods high in fat and carbohydrates. The National Health and Nutrition Examination Survey (NHANES) showed significantly higher rates of obesity in adults who reported an average of less than 7 hours of sleep a night. A chronic pattern of sleep duration of less than 6 hours a night has been associated with a higher body mass index (BMI). Short sleep duration is reportedly associated with higher energy intake, mainly due to increased consumption of saturated fat, poor eating habits, including an increase in meals, snacks, and night-time eating, with the consumption of high energy foods, lower intake of fruits and vegetables, and a higher intake of fast foods, sugar, and fats, resulting in an overall higher energy intake and increased BMI. (2) It is extremely important to monitor sleep quality throughout a medically assisted weight loss program. If your provider is concerned about your sleep quality, they will order a sleep study for a further analysis on what could be the problem. - Forgetting to take medications Your obesity medicine provider will prescribe you the medications that they believe will work best for you in promoting weight loss. If at any moment you have any problems with your medication, discuss them with your provider on your next visit so that they can find what medication is best for you. Some medications may lead to side effects, and it is important to communicate these concerns with your provider if they are bothersome. Skipping medication due to forgetfulness or due to lack of communication with your doctor may lead to unsuccessful results.
What is the difference between medical weight loss and any other type of weight loss treatment?
- Run by medical professionals
The first and biggest difference is that a medically assisted weight loss program is run by obesity medicine medical providers which can include physicians, nurse practitioners, physician’s assistants, nurses, dietitians, and health coaches. This allows for a safe environment of trusted professionals that will guide you along your weight loss journey. - One-on-one personalized experience
These trained professionals work one-on-one with patients to achieve real and long-lasting results. Weight loss, along with many things in life, cannot be achieved with a “one size fits all” approach. Fad diets, slim teas, detox cleanses, and other trendy weight loss solutions are expensive, restrictive, and difficult to maintain. These quick fixes are not created with the consideration of your personal weight loss needs, but rather a way to profit financially from individuals seeking quick solutions. The consideration of the individual and their needs is crucial to success in any effective weight loss solution. - Not a weight loss fad or trend
Weight loss fads and trends likely lead to short term and/or unsuccessful weight loss attempts. These unsuccessful attempts at losing weight undoubtedly lead to frustration, disappointment, and possibly even a loss of hope for future weight loss. Therefore, it is very important to find a weight loss solution that is personalized, attainable, and built for the long term.
How weight can affect health
Comorbidities
With small amounts of weight loss, patients begin to see improvement in glycemic measures and triglycerides. The relationship between weight loss and glycemia is one that is very close. This is great for diabetes prevention as it takes only small amounts of weight loss to prevent the progression of type 2 diabetes. Modest weight loss (5 to 10%) is also associated with improvement in systolic and diastolic blood pressure and HDL cholesterol. For some comorbid conditions, more weight loss is needed – 10% to 15% – to translate into clinical improvement such as with obstructive sleep apnea, and non-alcoholic steatotic hepatitis. Modest weight loss (5–10%) also leads to improvements in measures of quality of life, depression, mobility, sexual dysfunction, and urinary stress incontinence, and with further weight loss there are further improvements. (4)
Pain
Nearly half of Americans are projected to experience osteoarthritis of at least one knee in their lifetime. The excess physical burden of body weight can play a role, especially in lower extremity arthritis and pain. For example, in knee osteoarthritis, every pound of excess weight exerts a four-fold burden on the knee per step in daily activities. (4)
Prediabetes and Diabetes
An analysis by Hamman from the American Diabetes Prevention Program showed that in individuals with impaired glucose tolerance, for every kilogram of weight lost there was a 16% reduction in risk for progression to diabetes. Additionally, an average weight loss of 6.7% reduced the incidence of diabetes by 58% in the group participating in the American Diabetes Prevention Program and similarly in the Finnish Diabetes Prevention Trial. (4)
If you think that medical weight loss may be the right option for you, don’t hesitate to contact us here at Paragon Health Partners. We are here to help you find the best version of you.
FAQs
- Am I eligible for medically assisted weight loss?
If you are 18 or older with a BMI of 30 or above or a BMI of 27 or above with comorbidities, you may be eligible for medical weight loss.
- Is medical weight loss covered by insurance?
Due to legislature changes with the Affordable Care Act, insurance companies are required to provide obesity screening and treatment. This treatment may differ by state and insurance company, but this program is covered by most major insurance plans.
- Are medications for weight loss safe?
Possible side effects vary depending on each medication and how it acts on your body. Most side effects are mild and most often improve if you continue to take the medication. Rarely, serious side effects can occur. The FDA has approved five of these drugs—orlistat (Xenical, Alli), phentermine-topiramate (Qsymia), naltrexone-bupropion (Contrave), liraglutide (Saxenda), and semaglutide (Wegovy)—for long-term use. You can keep taking these medications as long as you are benefiting from treatment and not experiencing serious side effects. Sometimes health care professionals use medications in a way that’s different from what the FDA has approved, which is called “off-label” use. “Off-label” use is a standard practice in medicine, but make sure that you discuss any concerns or questions you may have with your medical provider.
- Do weight loss medications really work?
On average, after 1 year, people who take prescription medications as part of a lifestyle program lose 3% to 12% more of their starting body weight than people in a lifestyle program who do not take medication. Research shows that some people taking prescription weight management medications lose 10% or more of their starting weight. However, results vary by medication and patient. (3)
- Are weight loss medications covered by insurance?
Some, but not all, insurance plans cover medications that treat overweight and obesity. Contact your insurance provider to find out if your plan covers these medications.
- How long does the program last?
The program lasts as long as your medical provider sees fit. They will analyze at each visit how your progress is going and determine the length of treatment.
Visit our medically assisted weight loss page to learn more about how we can help you achieve your weight loss goals.
Citations
- Sinha, Rajita, and Ania M Jastreboff. “Stress as a common risk factor for obesity and addiction.” Biological psychiatry vol. 73,9 (2013): 827-35. doi:10.1016/j.biopsych.2013.01.032
- Papatriantafyllou, Evangelia et al. “Sleep Deprivation: Effects on Weight Loss and Weight Loss Maintenance.” Nutrients vol. 14,8 1549. 8 Apr. 2022, doi:10.3390/nu14081549
- Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: A systematic and clinical review. JAMA. 2014;311(1):74–86. doi:10.1001/jama.2013.281361
- Ryan, Donna H, and Sarah Ryan Yockey. “Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over.” Current obesity reports vol. 6,2 (2017): 187-194. doi:10.1007/s13679-017-0262-y
- “Prediabetes – Your Chance to Prevent Type 2 Diabetes.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 30 Dec. 2022




